Older Americans are living longer, working longer, and have undiminished desires to thrive and interact with their communities. In fact, 40% of America’s GDP is contributed to, by the 50+ age segment.*
Yet, everywhere from Hollywood to our healthcare systems, older adults are seen as decrepit dependents doomed to seclusion and decay. As witnessed in the latest Wisdo Health webinar held on October 26th, the reality is more optimistic and complex than the outdated stigma suggests.
“Aging is another word for living,” pointed out Annette Fellows, Vice President of Health Products & Services at UnitedHealthcare, as she and Dr. Charlotte Yeh, Chief Medical Officer of AARP Services, explained how a Personal Determinants of Health (PDoH)-centered care strategy can actually lead to improved health outcomes and lower medical costs among older adults.

Impacts of Ageism and the Welcomed Paradigm Shift of the Hundred-Year Life
The discussion began with compelling points raised by Dr. Charlotte Yeh on the prevalence of ageism in our culture, and even in our healthcare systems, with devastating results. As Dr. Yeh so eloquently stated, “Just because you’re over 65, does not mean you aren’t worthy of a better life for tomorrow, and it’s affecting how healthcare is delivered.”
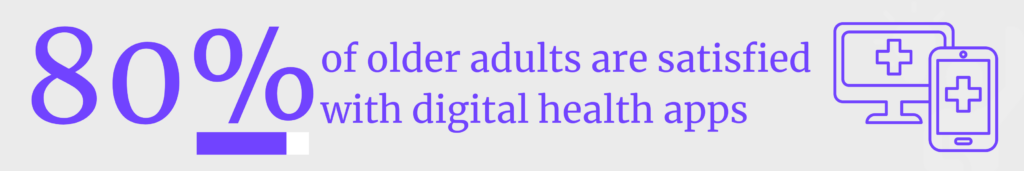
This is particularly prevalent in the case of referrals to digital health apps. Dr. Yeh provided stats from the UK where, despite many of these platforms being a cost-effective way to bolster independence and ease PDoH-related challenges, and that 80% of older adults are satisfied or very satisfied with the use of digital health apps, “only one in 25 patients 55 and older will be recommended a digital health app. And if you are 65 and older, it drops to one in 50.”*
Dr. Yeh also cited a recent AARP survey with older adults, which found that 80% of older adults experience at least one form of ageism in their everyday lives.
Yet, maintaining a positive outlook on aging is essential. Not only does it affect quality of life, as detailed below, but it also affects the bottom line of health insurance providers.
“There is a $63 billion annual cost due to ageism in our healthcare system.*
So how can we adjust our approach to aging in healthcare to reflect the realities of aging today?
It begins with acknowledging the impact of personal determinants of health on overall health and medical costs.
PDoH As the Third Lever for Improved Health
From here, Annette Fellows discussed levers for improved health in older populations.
“As we care for our members, we are looking at three levers of care or improved health”: healthcare determinants, social determinants, and personal determinants.
“It is not just healthcare or social determinants. It’s those two plus personal determinants,” illustrating an additional point by Mrs. Fellows: “80% of what determines health occurs outside of the healthcare system and health determinants.”*
So, what does determine our health, particularly as we age?
Mrs. Fellows pointed out that, “as protective factors—or positive resources—like resiliency, purpose, optimism, social connection, and locus of control increase, negative outcomes related to perceived stress, depression, health status, functionality, decrease.
The more positive factors there are, the larger the decrease in negative outcomes one will experience. In fact, each additional protective factor is associated with an incremental $1,356 reduction in medical costs.*
The 3 P’s and the Business Case for Addressing PDoH in Healthcare Strategy
UnitedHealthcare and AARP Services have summarized PDoH in what they call the Three Ps: purpose, possibilities (i.e., optimism), and people.
Individuals with a sense of purpose have:*
- 71% reduced risk of stroke
- 58% better sleep
- 39-61% fewer overnight hospitalizations
- 18-32% fewer doctor visits.
Those with a positive view of aging:*
- Are 44% more likely to recover from a severe disability
- have an 80% reduction in cardiovascular risk
- live up to 7.5 years longer.
The third factor, “people,” is particularly fascinating for Wisdo Health and the greater loneliness awareness community, as the data is presented in the context of loneliness, which:*
- shaves eight years off of longevity.
- has the largest negative effect on quality of life, and
- is the single largest predictor of dissatisfaction with healthcare.
- Results in higher mortality rates than obesity.
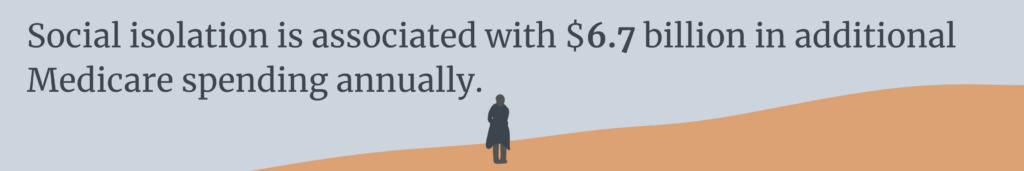
Social isolation among older adults is associated with 6.7 billion in additional Medicare spending annually*
As ageism becomes recognized as an obstacle to health equity, healthcare will then be able to more effectively address the needs of aging populations in the next chapter of their journey, making way for care that is effective and cost-effective, as well.
We hope that you will join us for our next webinar, which will be hosted by Bright Spots in Healthcare on November 17, 2022 at 12 pm ET. Wisdo’s CEO and Founder, Boaz Gaon, will be joined by Mike Franz, MD, Senior Medical Director of Behavioral Health, Regence, Lisbeth Briones-Roberts, Chief Togetherness Officer at SCAN Health Plan, and Jennifer Spear, Associate Director, Population Health at Humana for yet another fascinating conversation on Peer Support to Improve Medicare Advantage Outcomes. Attendance is free.
*Sources:
- “The Longevity Economy® Outlook” AARP (2019) and “Entrepreneurial Demographics, National” Kauffman Foundation (2014); *Source: https://orchahealth.com/wp-content/uploads/2021/07/2107_ICS_Research_Report_2021_National_final.pdf
- Becca R Levy, PhD, Martin D Slade, MPH, E-Shien Chang, MA, Sneha Kannoth, MPH, Shi-Yi Wang, MD, PhD, Ageism Amplifies Cost and Prevalence of Health Conditions, The Gerontologist, Volume 60, Issue 1, February 2020, Pages 174–181, https://doi.org/10.1093/geront/gny13;
- https://www.ncsl.org/portals/1/documents/health/HealthDisparities1213.pdf
- Hill, P. L.,Turiano, N. A.,Mroczek, D. K., & Burrow, A. L. (2016). The value of a purposeful life: Sense of purpose predicts greater income and net worth. Journal of Research in Personality,65, 38-42. doi:10.1016/j.jrp.2016.07.003
- Becca R Levy, PhD, Martin D Slade, MPH, E-Shien Chang, MA, Sneha Kannoth, MPH, Shi-Yi Wang, MD, PhD, Ageism Amplifies Cost and Prevalence of Health Conditions, The Gerontologist, Volume 60, Issue 1, February 2020, Pages 174–181, https://doi.org/10.1093/geront/gny131
- Musich, S., Wang, S. S., Schaeffer, J. A., Kraemer, S., Wicker, E., & Yeh, C. S. (2020). The additive impact of multiple psychosocial protective factors on selected health outcomes among older adults. Geriatric Nursing. doi:10.1016/j.gerinurse.2020.09.007